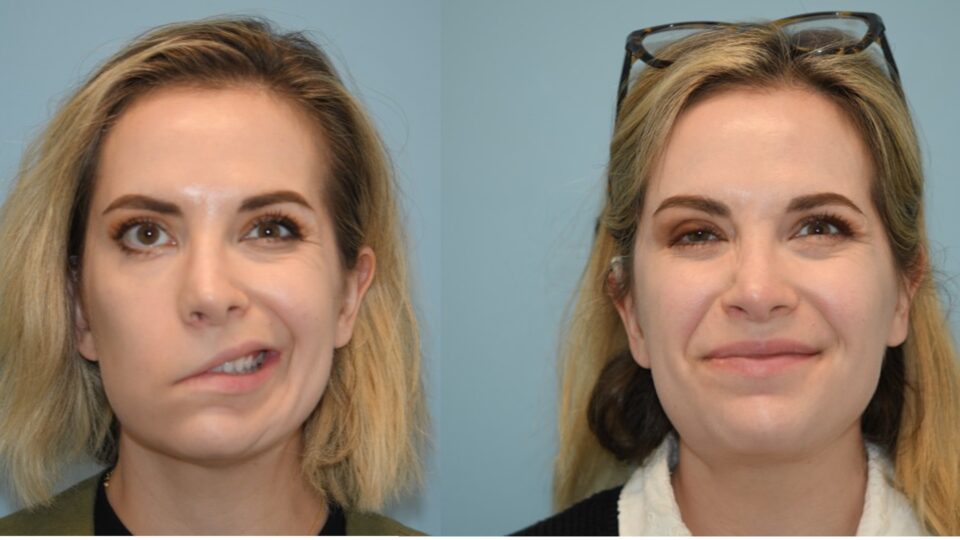
Acclaimed endoscopic skull base surgeon Carlos D. Pinheiro Neto, MD, PhD, has joined NYU Langone Health as vice chair of otolaryngology—head and neck surgery.
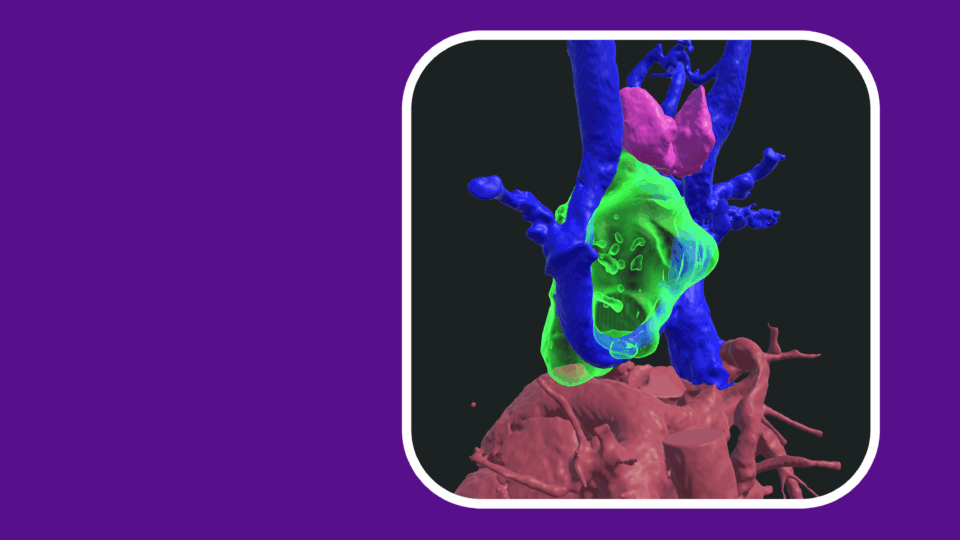
Dr. Pinheiro Neto has contributed to minimally invasive surgical techniques that use small endoscopes and the nostrils as a corridor to reach intracranial tumors, avoiding the need for large facial incisions or craniotomies. At NYU Langone, Dr. Pinheiro Neto will continue his extensive research in the anatomy lab to advance less invasive methods for resecting benign and malignant tumors of the nose, sinuses, and skull base, focusing on safeguarding nasal and sinus structures and maximizing patients’ quality of life after surgery.
Previously, Dr. Pinheiro Neto served as a professor of otolaryngology—head and neck surgery at Mayo Clinic in Rochester, Minnesota, where he also directed the fellowship in skull base surgery and rhinology.
Here, he reflects on the success of free mucosal grafts in pituitary surgery, introduces his work on the nasal septum free flap, and explores AI-supported referrals to expand access to endoscopic skull base surgery.
Physician Focus: Of the many techniques you’ve contributed to over the past decade, which stands out for its impact on the field?
Dr. Pinheiro Neto: I have a PhD in anatomy and I am passionate about developing innovative surgical approaches in the lab that translate to the operating room to improve skull base surgery. One advancement I’m particularly excited about is the growing use of the free mucosal graft in pituitary tumor surgery reconstruction.
Pituitary tumors are typically removed through the nose during endoscopic transnasal transsphenoidal surgery. A major concern after removing pituitary tumors is postoperative cerebrospinal fluid (CSF) leaks—fluid from the brain dripping through the nose. When these occur, patients often require one or more surgeries to repair the leaks. It’s very concerning, because leaks can lead to life-threatening meningitis.
“I have a PhD in anatomy and I am passionate about developing innovative surgical approaches in the lab that translate to the operating room.”
Carlos Pinheiro Neto, MD, PhD
The standard procedure to prevent potential CSF leaks when there is a high-flow intraoperative CSF leak during a pituitary surgery is using nasoseptal flaps created from the septum. But nasoseptal flaps can cause trauma to the nose, a structural collapse in the nasal bridge, and an increased risk of septal perforations.
In the anatomy laboratory, we studied the free mucosal graft as an alternative reconstructive technique. This technique uses grafts from the nasal floor to provide a seal between the nose and brain after tumor removal. In our 2019 study in World Neurosurgery, conducted with colleagues at Albany Medical Center, we reported a 0.82 percent postoperative CSF leak rate with free mucosal graft reconstruction, compared to 7.4 percent without reconstruction. The reported postoperative CSF leak rate for the nasoseptal flap ranges from 0 to 2.9 percent.
Since changing our paradigm from the nasoseptal flap to the free mucosal graft for pituitary tumor surgery, we’ve reduced our CSF leak rate in pituitary surgery to just 0.2 percent.
Physician Focus: What are some innovative procedures you’re currently developing?
Dr. Pinheiro Neto: One technique we’re developing is the nasal septum free flap for laryngeal reconstruction, in which the nasoseptal flap with the cartilage attached is harvested and removed from the nose with its blood vessel. The blood vessel is then sutured to a vessel in the neck and the flap is used to reconstruct the larynx. It’s currently in development in a porcine model. I am also investigating ways to remove brain tumors through the nasal corridor while preserving olfaction.
“I’m excited to work at NYU Langone, one of the top health systems in the country, and in New York City, which offers a large patient referral base.”
Physician Focus: Will you be expanding those research areas at NYU Langone?
Dr. Pinheiro Neto: Yes, I’m looking forward to expanding these research areas and working with head and neck surgical oncologist Umamaheswar Duvvuri, MD, PhD, at Perlmutter Cancer Center, as well as neurosurgery and research fellows in the NYU Langone anatomy lab. Together, we aim to apply our less invasive endoscopic skull base surgery techniques to more patients, especially in highly complex cases.
Physician Focus: What do you consider to be the biggest challenges ahead in the field of endoscopic skull base surgery?
Dr. Pinheiro Neto: One of our biggest challenges is reaching more patients who could benefit from our techniques. I’m eager to work with NYU Langone’s AI team to develop an algorithm-driven patient referral process that identifies patients likely to need sinus surgery. I’m excited to work at NYU Langone, one of the top health systems in the country, and in New York City, which offers a large patient referral base.