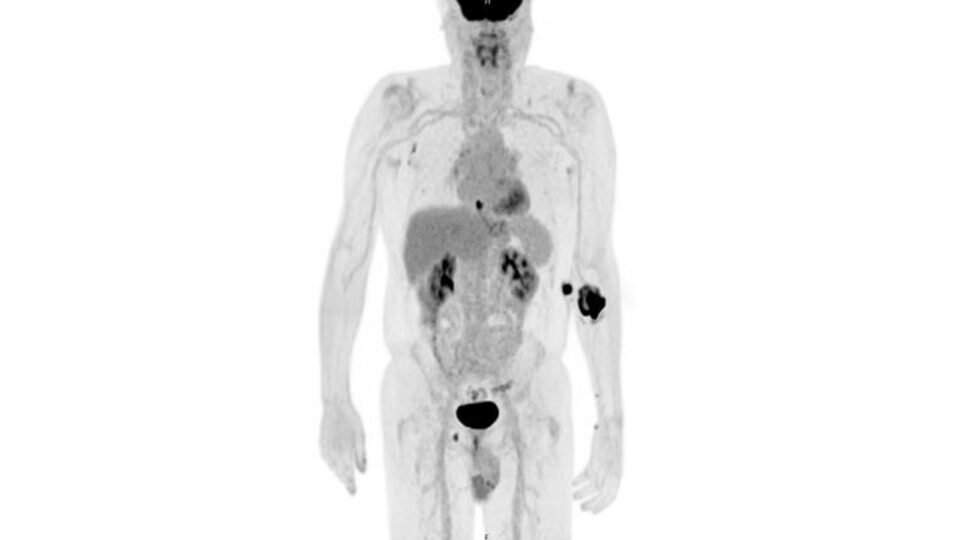
A 66-year-old male recently presented to NYU Langone Health with a localized lung tumor in the right middle lobe at high risk for malignancy. During surgery to resect the tumor, it was discovered to involve a hilar lymph node and extend into the main pulmonary artery.
Despite the complexity—including a pulmonary artery sleeve resection—thoracic surgeon Michael Zervos, MD, and team performed the entire procedure robotically. Dr. Zervos’s expertise in robotic vascular control, particularly in managing the pulmonary artery, was central to the case’s success.
“It was thought a sleeve of the pulmonary artery could only be safely done through open techniques. But with the refinements of robotic technology, it is absolutely doable,” says Dr. Zervos.
Driven to Innovate
Recalling the procedure, Dr. Zervos explains, “Initially, I thought I could get the tumor off the pulmonary artery. But when I saw the tumor was in the lymph node that was then adherent to the pulmonary artery, I realized there would be no way for me to remove all of the cancer without removing the artery as well.”
“As advanced as imaging is today, there is still an element of surprise when you get to the operating room. And the question is, how do you deal with that?”
Michael Zervos, MD
At that point, he turned to his robotic vascular tray, a set of instruments he has prepared for any high-risk procedure. Among them were bulldog clamps, which he used to temporarily cut off blood flow to the impacted section of the pulmonary artery.
Dr. Zervos then excised the affected tissue and performed artery reanastomosis using a Gore-Tex suture, having determined that its handling pairs well with the robotic instrumentation. “The pulmonary artery is especially delicate, because it lacks a layer of tissue that most arteries have, making the suturing more challenging,” he notes.
At NYU Langone, even the most innovative robotic surgeries commonly maintain the institution’s short length of stay, and this case was no exception—the patient was discharged home just one day after surgery, with minimal pain and no limitations to his activities.
It’s now been eight months since the procedure, and the patient remains cancer free.
Medical oncologist Abraham Chachoua, MD, is overseeing the patient’s adjuvant chemotherapy with immunotherapy.
“As advanced as imaging is today, there is still an element of surprise when you get to the operating room. And the question is, how do you deal with that?” says Dr. Zervos. “This case speaks to our flexibility, experience, and comfort level in addressing a difficult problem when it’s encountered intraoperatively—without converting to an open thoracotomy.”