A comprehensive single-cell RNA sequencing analysis of immune checkpoint expression in human atherosclerotic plaques has revealed how cancer immunotherapies may accelerate cardiovascular disease. The findings, recently published in Nature Cardiovascular Research, offer new insights into designing immune checkpoint inhibitors (ICIs) that reduce cardiovascular complications.
“Our findings are that it is critical to consider how cancer treatments like immune checkpoint inhibitors can affect cardiometabolic risk,” says Kathryn J. Moore, PhD, the Jean and David Blechman Professor of Cardiology and the director of NYU Langone Health’s Cardiovascular Research Center.
“It is critical to consider how targeting cancer treatments … can affect cardiometabolic risk.”
Kathryn J. Moore, PhD
Dr. Moore co-led the study alongside Chiara Giannarelli, MD, PhD, associate professor in the Leon H. Charney Division of Cardiology.
CCR7+FSCN1+ Dendritic Cells: A Central Hub
In patients treated with ICIs, immune-related adverse events (irAEs) are common and often necessitate discontinuation. When focusing on irAEs affecting the heart, past studies have shown that approximately 10 percent of patients undergoing ICI treatment experience a major adverse cardiovascular event (MACE). However, the underlying mechanisms remain unclear.
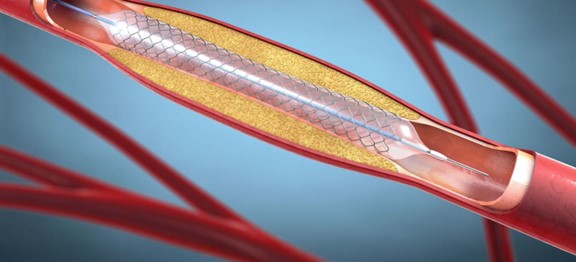
To explore this issue, the research team led by Dr. Moore and Dr. Giannarelli investigated how immune checkpoint inhibitors, drugs which reactivate T cells to kill cancer cells, interact with immune cells within arterial plaques.
Using single-cell RNA sequencing of immune cells from atherosclerotic plaques—either carotid or coronary—the researchers determined that most T cells within these plaques can be directly influenced by FDA-approved ICIs targeting PD-1, CTLA-4, and LAG3.
Notably, CCR7+FSCN1+ dendritic cells, similar to those found in the tumor microenvironment, were identified as key mediators of the immune response to ICIs within plaques.
These cells, which make up about 0.7 percent of plaque myeloid cells, express multiple checkpoint molecules targeted by approved and investigational cancer therapies. The researchers found that this cell type became more prevalent following PD-1 or CTLA-4 inhibition. And their cell responses were linked with T cell activation, enhanced cytotoxity and proliferation—key players in the pathogenesis of atherosclerosis.
“Our findings provide new insight into how a class of drugs intended to reactivate immune response to tumors can also prompt a heightened immune response in arteries.”
Chiara Giannarelli, MD, PhD
“Our findings provide new insight into how a class of drugs intended to reactivate immune response to tumors can also prompt a heightened immune response in arteries and increase risk of heart disease,” says Dr. Giannarelli.
T2D and Lipid-Lowering Reshapes Checkpoint Landscape
The investigators also explored how type 2 diabetes, a known risk factor for both cancer and heart disease, may make those with atherosclerosis even more vulnerable to irAEs.
As part of the study, the team assessed immune checkpoint expression in arterial tissue collected from patients both with or without diabetes. The results showed that in patients with diabetes the communication between immune cells, mediated by immune checkpoints, is reduced. The decrease of this brake on the immune system can prompt increased inflammation and cardiovascular disease risk in diabetes.
Other experiments further revealed that lipid-lowering therapies commonly prescribed in patients to reduce plaque buildup and inflammation can restore beneficial immune cell communications. Indeed, the researchers’ experiments in rodents confirmed that such lipid lowering boosts communication between immune checkpoints within atherosclerotic arteries, thereby reducing plaque inflammation. In patients with cancer the anti-inflammatory benefits of fat reduction may mitigate the negative effects of blocking immune checkpoints.
Shaping Safer ICIs
Collectively the work sets the stage for designing ICI strategies that minimize cardiovascular disease risk in survivors of cancer.
The authors also say that building comprehensive maps of the immune checkpoint interactome in other organs or disease states is an important next step in designing ICI treatments that reduce irAEs.
“Now that we have a better understanding of the interplay between these diseases,” says Dr. Moore, “we can begin to explore new strategies to lower the risk of unintended health concerns caused by their treatment.”