NYU Langone Health is one year into a pilot study exploring phage therapy as a potential treatment for intractable nontuberculosis mycobacteria (NTM) infections.
A significant number of patients with underlying bronchiectasis develop severe chronic NTM infection that’s refractory to even the most aggressive antibiotic regimens. With limited treatment options, these patients can develop fibrosis and cavitary lung disease, sometimes necessitating lung transplantation—an option further complicated by the ongoing NTM infection.
As the largest member of the COPD Foundation’s Bronchiectasis and NTM Research Registry, NYU Langone is a leader in NTM research and treatment, nationally recognized as a referral center for bronchiectasis, NTM infections, and cystic fibrosis.
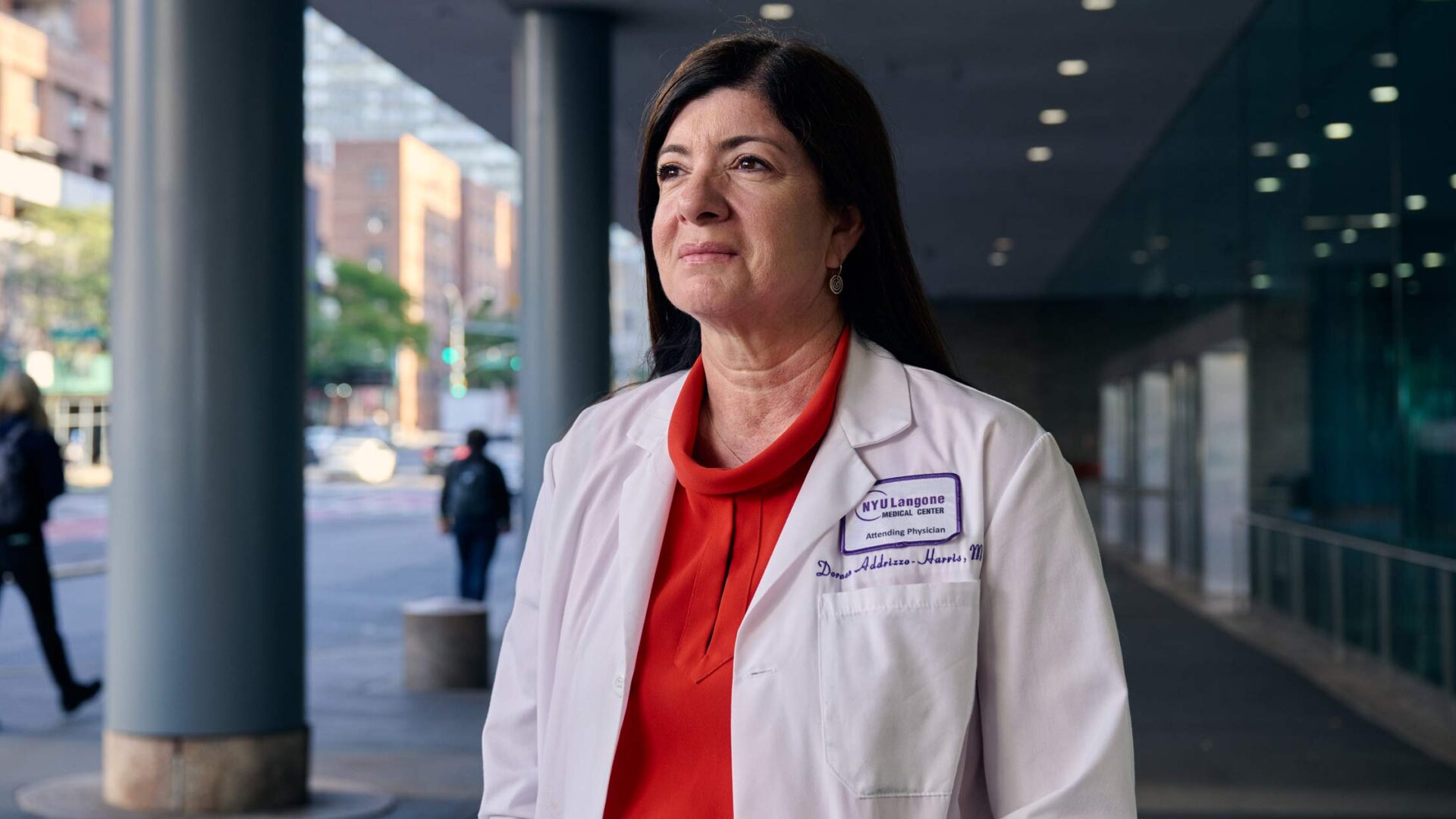
Here, acclaimed pulmonologist Doreen J. Addrizzo-Harris, MD, director of NYU Langone’s Bronchiectasis and NTM Program, highlights the collaborative research initiative, the therapeutic potential of phage therapy, and her partnership with the COPD Foundation on a long-term vision for national phage research.
Physician Focus: What do we know about the potential advantages phage therapy might offer over traditional antibiotic therapies for NTM infections?
Dr. Addrizzo-Harris: Phage therapy offers several potential advantages for managing NTM infections. For one, they can kill the antibiotic-resistant strains that underlie refractory cases. They can also work synergistically with antibiotics, potentially restoring bacterial susceptibility to these drugs. Phages are also highly specific, effectively preserving the patient’s microbiota while eliminating just the targeted pathogenic bacteria. Additionally, they have a favorable safety profile. All of this makes phage therapy a promising adjunct or alternative in cases of treatment failure.
Physician Focus: What led you to explore phage therapy as a potential treatment for patients with chronic NTM infections?
Dr. Addrizzo-Harris: In 2023, a 20-case series published in Clinical Infectious Diseases on phage therapy for patients with drug-resistant NTM lung disease found that over 50 percent of patients showed some improvement. The therapy was also shown to be safe, with no adverse reactions attributed to it. That spurred on our research.
We began consulting with Graham Hatfull, PhD, who led the study, and his team at the University of Pittsburgh to obtain the phages to be used in potential patients at our center. We’re also consulting with physician-scientists, including Jerry Nick, MD, a fellowship-trained pulmonologist at National Jewish Health who specializes in cystic fibrosis and bronchiectasis in adults, for their research protocols.
Physician Focus: You’re one year into the planning and initial recruitment. Can you tell us about the study design and what you hope to learn?
Dr. Addrizzo-Harris: We’re starting with the most severe cases of our patients with NTM infection and underlying bronchiectasis. These patients are progressing, some despite years of intravenous antibiotics and surgery. We’re hopeful it may give them a better quality of life, even if it’s just for a few years.
“We’re hopeful it may give them a better quality of life, even if it’s just for a few years.”
Doreen Addrizzo-Harris, MD
Phage therapy can be nebulized, but in our study, patients will be self-administering a daily intravenous phage, formulated by the pharmacy, along with their antibiotic therapy. Many of these patients are already on IV antibiotics, so they already have an indwelling port or a PICC line. Our plan is for patients to continue phage therapy for a year, then we’ll evaluate.
We’re hoping to enroll a number of patients over the next two to three years. Fellow Alexandria Imperato, MD, who will be staying on as an attending physician, will be a study co-principal investigator with me. We will be collaborating with Leo Segal, MD, director of the Lung Biology Laboratory at NYU Langone, to investigate biomarkers in these patients at the microbiome level.
Physician Focus: How will recruitment for your study work?
Dr. Addrizzo-Harris: We are looking at our current patients to see who qualifies. Phage therapy is an unapproved research therapy. To be used in our study, there’s a matching process. Not all patients with NTM infection will have an isolate match at a phage biobank that can kill the majority of the mycobacterium. For each qualified patient with a match, we will submit a single-patient Investigational New Drug (IND) application. Each phage requires individual FDA approval for each patient.
For our first effort, three of the four qualified patients have phage matches that seem to be effective. If these phages get FDA IND approval, we hope to start with phage therapy for these patients this summer.
Physician Focus: How could phage therapy impact the treatment approach for patients with persistent NTM infections?
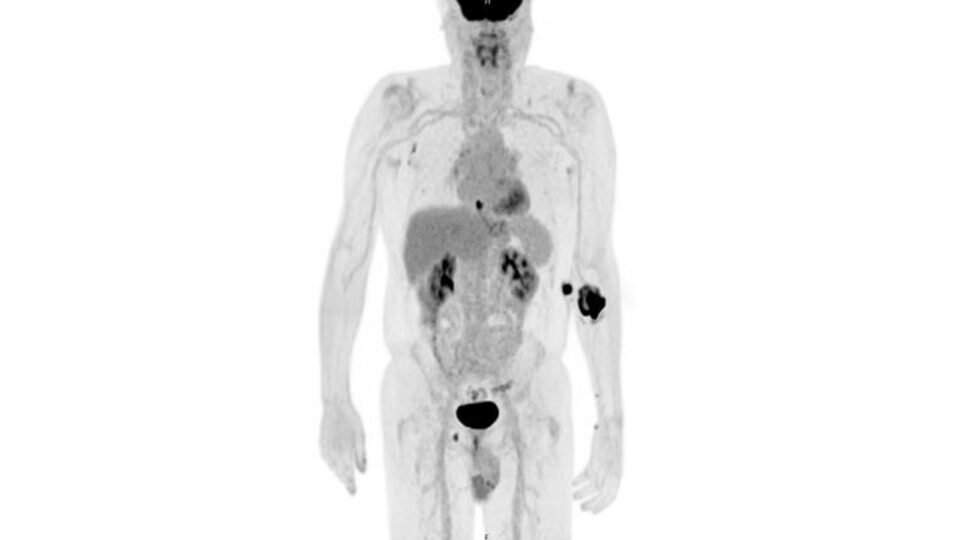
Dr. Addrizzo-Harris: Phage therapy won’t allow these patients to discontinue antibiotic therapy, but it may allow us to change them from intravenous to oral antibiotics, which would make their lives much easier, and give them a lower level of oral antibiotic therapy. Overall, we hope phage therapy will reduce the burden of disease so that antibiotic therapy will be able to prevent disease progression, based on either culture results showing that the disease has decreased, or by monitoring CT scan results. Patients with a negative culture could also then be a candidate for lung transplant.
“If we can show with two, three, or four additional patients that phage is safe, effective, and can be easily administered, then we might be able to get federal or industry resources to conduct a large trial.”
We’re just at the beginning of our research, but it’s extremely exciting because these patients with persistent NTM infection have no other treatment options.
Physician Focus: What are the key barriers to making bacteriophage therapy a viable clinical option for NTM infections?
Dr. Addrizzo-Harris: For phage therapy to really take off, we will need much larger prospective randomized trials. But right now, our goal is to try and do a series of these cases to bring more data to the forefront. If we can show with two, three, or four additional patients that phage is safe, effective, and can be easily administered, then we might be able to get federal or industry resources to conduct a large trial.
Moving forward, the COPD Foundation has created a new subsidiary, the Bronchiectasis and NTM Association. As part of this new subsidiary, I am chairing an initiative that has named NYU Langone the first of 33 Centers of Excellence across the country. We hope to eventually have 150 of these centers in our clinical care network. Our goal is to collaborate on our clinical trials to potentially have a multicenter phage trial, and other trials for patients with mycobacterium, that won’t necessarily be dependent on industry for research funding.