When a 20-month-old female was diagnosed with the extremely rare genetic disorder RHOBTB2-Related Disorder (RD)—with just a few dozen confirmed cases at the time of her diagnosis in 2022—her care team turned to the available literature to plan a tailored treatment strategy. Combining carbamazepine with intensive multidisciplinary rehabilitation, they set their sights on restoring her mobility and supporting her journey toward normal development.
The young female had been followed for frequent stiffening episodes with concerns for seizures by NYU Langone Health’s Comprehensive Epilepsy Center. Because of her developmental delays, including speech and challenges walking, as well as painful dystonic episodes, she was referred to neurogenetics specialist Nicolas J. Abreu, MD, associate director of NYU Langone’s Division of Neurogenetics.
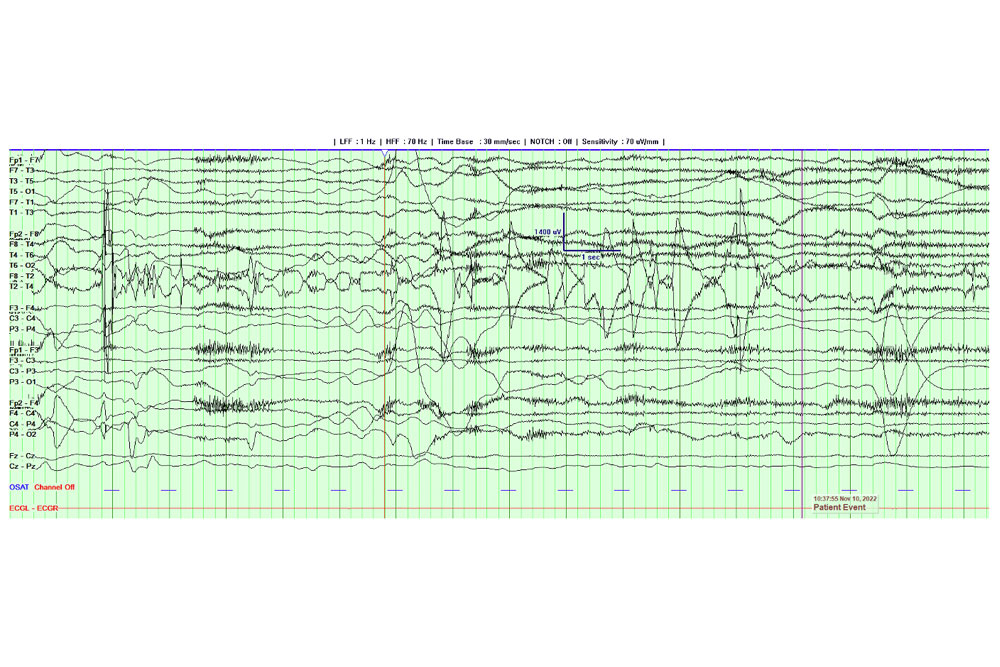
Dr. Abreu reasoned that for such severe episodes and global developmental delay, comprehensive genetic testing was appropriate, especially given that a brain MRI was normal and there was no evidence of seizures on EEG.
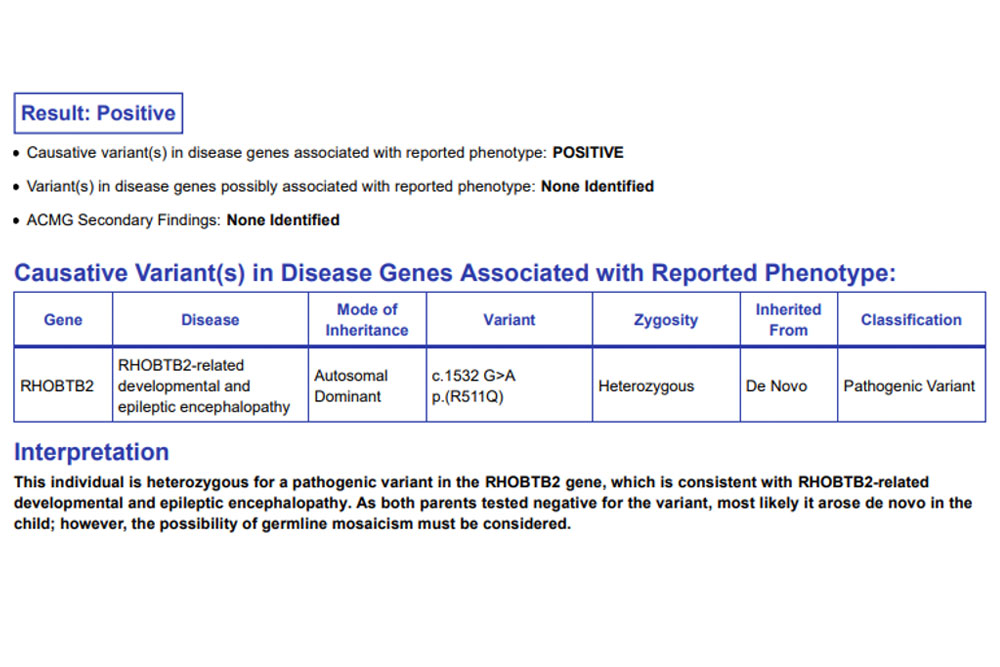
“We had already ruled out epilepsy, but given the neurodevelopmental delays and abnormal movements, I felt that broad genomic testing was needed,” Dr. Abreu explains. “Whole exome sequencing confirmed the diagnosis of RHOBTB2-RD, an exceptionally rare disorder, with fewer than 200 cases reported to date.” Movement disorders are common in this genetic disorder, he says, supporting that the patient’s frequent non-epileptic episodes were due to dystonia.
Case Highlights:
- The patient’s RHOBTB2-RD phenotype included global developmental delays and painful non-epileptic dystonia.
- Advanced genetic sequencing and expert interpretation from the Division of Neurogenetics were crucial for the diagnosis.
- Oral carbamazepine reduced dystonia episodes from 10 to a maximum of 4 a day.
- Early genetic testing should be considered for pediatric patients with severe, recurrent abnormal movements, regardless of epilepsy status.
Next-Gen Sequencing: A Path to Answers
RHOBTB2-RD, first described in 2018, is an ultrarare genetic disease with a highly heterogenous phenotypic spectrum. Patients may present with or without epilepsy, developmental delay, hemiparesis, movement disorders, or microcephaly.
Upon identifying the need for genomic testing, Dr. Abreu and the genetic counselor Connolly Steigerwald, MS, CGC, met with the patient and her family to discuss the latest genomic sequencing technologies and their clinical applications.
“Whole exome sequencing confirmed the diagnosis of RHOBTB2-RD, an exceptionally rare disorder, with less than 200 cases reported to date.”
Nicolas J. Abreu, MD
“Appropriate genetic testing should be performed for children with neurodevelopmental disabilities, including those with hyperkinetic movement disorders,” says Dr. Abreu. Moreover, for this patient population, exome or genome sequencing should be offered as first-tier tests. These services are available through NYU Langone’s Division of Neurogenetics in collaboration with Clinical Genetic Services.
“Pediatric neurologists may only be comfortable interpreting small, panel-based tests that include only a few hundred genes,” Dr. Abreu says. “We can analyze more than 20,000 genes using genomic next generation sequencing technologies like exome and genome.”
A Rare Case for Treatment
Coming up with a treatment plan for the patient was far from routine, notes Dr. Abreu, since the patient’s phenotype—characterized by global developmental delay and episodes of painful dystonia—was not well documented in the literature.
After reviewing the primary research, Dr. Abreu uncovered that certain cases of RHOBTB2-RD, particularly those with dystonia and global developmental delay, may respond to carbamazepine. Evidence from a case series of 11 pediatric patients found carbamazepine to be the most commonly used drug, having been administered to 7 patients. It was deemed beneficial in at least two of these cases.
Dr. Abreu collaborated with pediatric movement disorder specialist Claire Miller, MD, PhD, and a multidisciplinary team to plan a multimodal intervention that included oral carbamazepine (100 mg, twice a day) and intensive outpatient rehabilitation through Rusk Rehabilitation.
“I was cautiously optimistic,” Dr. Abreu recalls about the treatment decision. “Despite the limited reports available, carbamazepine has been used to treat movement disorders in other rare genetic conditions.”
Rapid Improvement
In the months that followed, the intervention greatly reduced the patient’s dystonic episodes—from 10 times a day to 4 at most, Dr. Abreu says. Occupational therapy, physical therapy, and speech therapy aided her movement and developmental progress, he added.
Remarkably, one week before her third birthday, the patient began to stand independently and to walk without assistance. “She is improving rapidly and is well on her way to recovery,” Dr. Abreu says.
The patient practicing to stand independently. Shared with permission from the family. Source: NYU Langone Health.
For similar diagnoses, Dr. Abreu encourages pediatric neurologists to explore genetic testing early in a child’s diagnosis for recurrent, severe abnormal movements, regardless of what the EEG shows. In this case, having access to appropriate genetic testing—and expert interpretation—was key to establish the diagnosis.
With respect to treatment, he recommends a thorough review of the literature, emphasizing that appropriate prescribing may be off-label for rare genetic movement disorders.