We recently made an uncommon diagnosis: a recurrent midline prostatic cyst causing partial ejaculatory duct obstruction and infertility. The patient had severe oligoasthenozoospermia and reported ejaculatory symptoms of delayed, uncomfortable, and low-volume ejaculate. While cyst aspiration at another center temporarily alleviated the ejaculatory symptoms, they quickly returned.
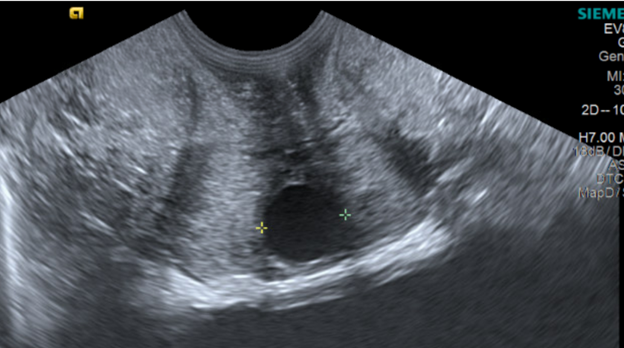
At our office, transrectal sonography confirmed the cyst’s recurrence, prompting a successful transurethral resection of the ejaculatory ducts (TURED).
This Case of the Month highlights the rare but treatable nature of midline prostatic cysts as a cause of male infertility, with properly performed TURED offering significant symptom relief and improved fertility outcomes.
Case Highlights:
- The 28-year-old male presented with fertility concerns and ejaculatory symptoms, with a history of an aspirated midline prostatic cyst and bilateral varicoceles.
- Given that cyst aspiration is not definitive, and varicoceles could not explain all symptoms, we suspected cyst recurrence, confirmed by imaging.
- TURED and bilateral microsurgical varicocelectomy were performed without complication.
-
Ejaculatory symptoms resolved immediately postsurgery; semen analysis at 10 months showed sustained success, with normal ejaculate volume and near-normal semen parameters.
Case Presentation
The 28-year-old male presented to our clinic for evaluation and management of ejaculatory pain and male infertility. He complained of chronic low-ejaculate volume and post-ejaculatory pain. Previous evaluation for male fertility concerns and painful ejaculation had shown low sperm count and motility, as well as abnormal morphology.
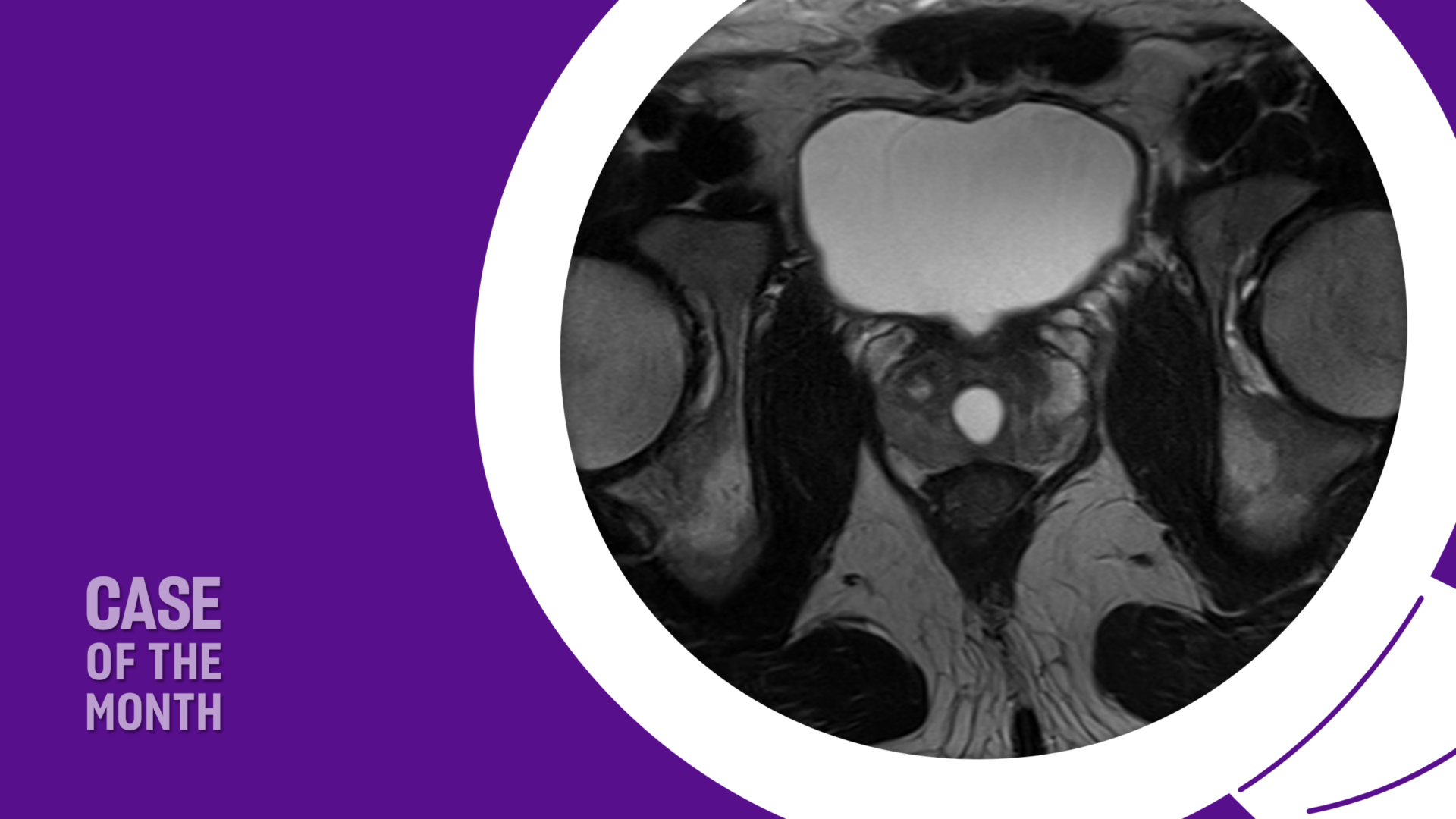
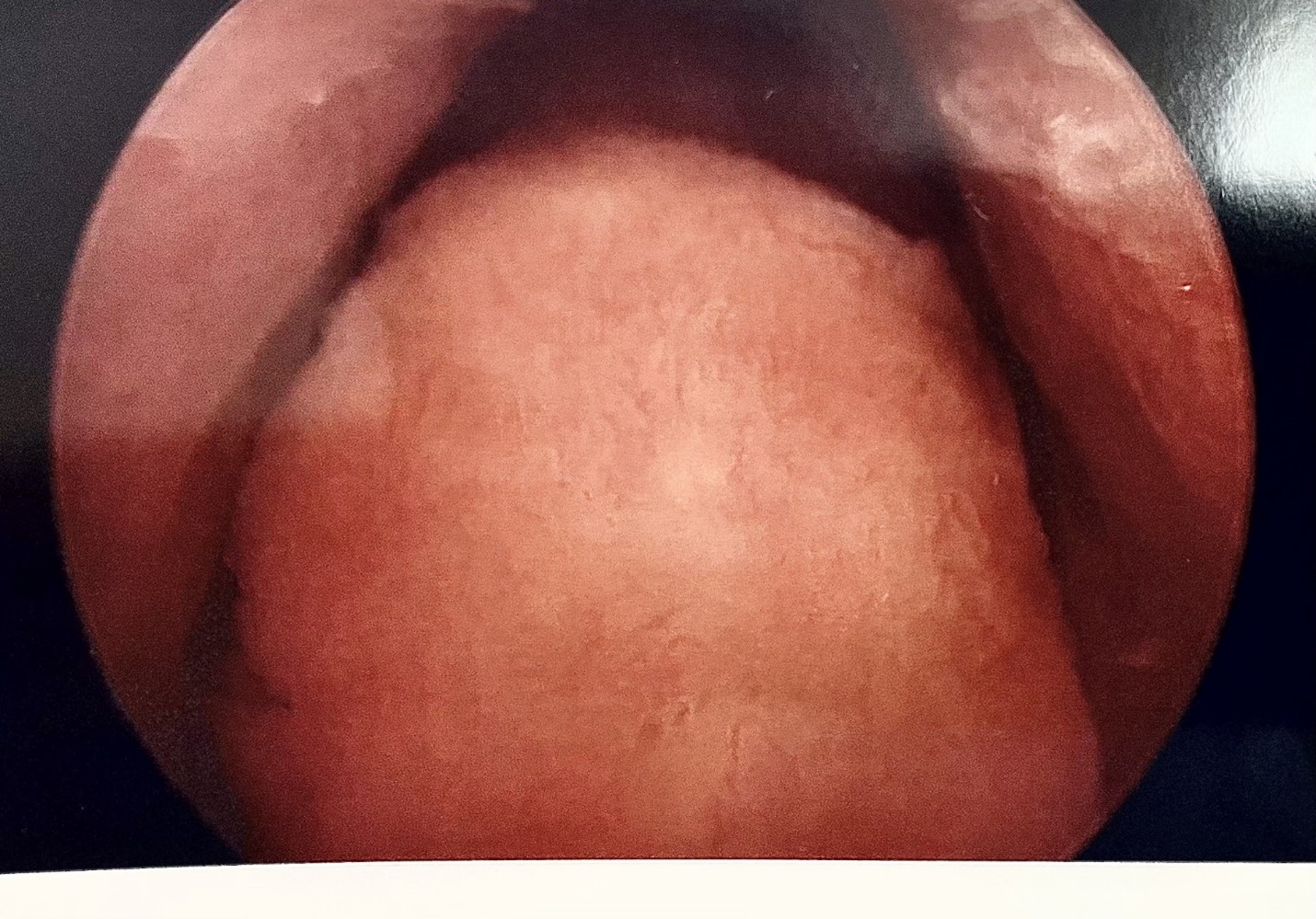
A prostate MRI one year prior to his visit revealed a 19-cc prostate with a midline cyst measuring 1.9 cm × 1.5 cm × 1.3 cm (Figure 1). The patient had undergone cyst aspiration under ultrasound guidance. This resulted in a transient improvement in ejaculate volume and resolution of peri-ejaculatory pain.
Within three months, the patient developed recurrent symptoms with low-ejaculate volume and pain after ejaculation.

Medical Examination
| Physical Exam—Genitourinary | Findings |
| Penis | Normal circumcised appearance, no lesions or palpable plaques. Glans without hyperemia, normal meatus. |
| Epididymis | Non-tender bilaterally. No evidence of fullness. |
| Testis | Palpable in dependent scrotum bilaterally symmetric. Both slightly small (15 to 20 cc), no masses palpable. |
| Vas Deferens | Palpable bilaterally. Left grade 3 varicocele. Right grade 1 varicocele |
| Labs | Results |
| Semen Analysis | |
| Volume | 1.4 mL (low; no collection issues) |
| pH | 8.2 |
| Concentration | 4 million/cc (low |
| Motility | 14% (low) |
| Morphology | 2% (low) |
| Follicle-stimulating hormone (FSH) | 4.8 (normal) |
| Testosterone | 679 ng/dl (normal) |
Diagnosis and Management
Varicoceles may result in abnormal semen parameters. However, the resurgence of painful and low-volume ejaculate suggested a recurrence (refilling) of the prostatic cyst as the cause of the patient’s symptoms, as cyst aspiration is typically not definitive.
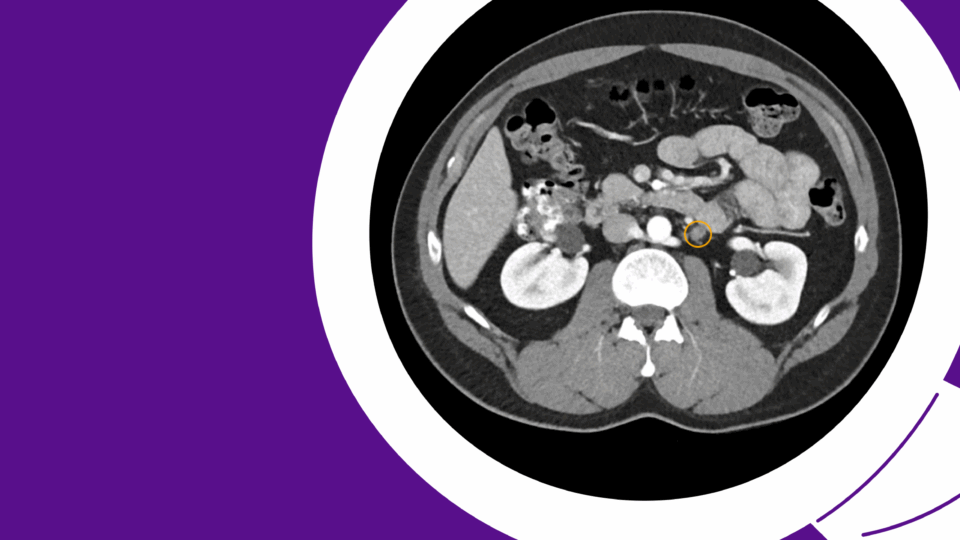
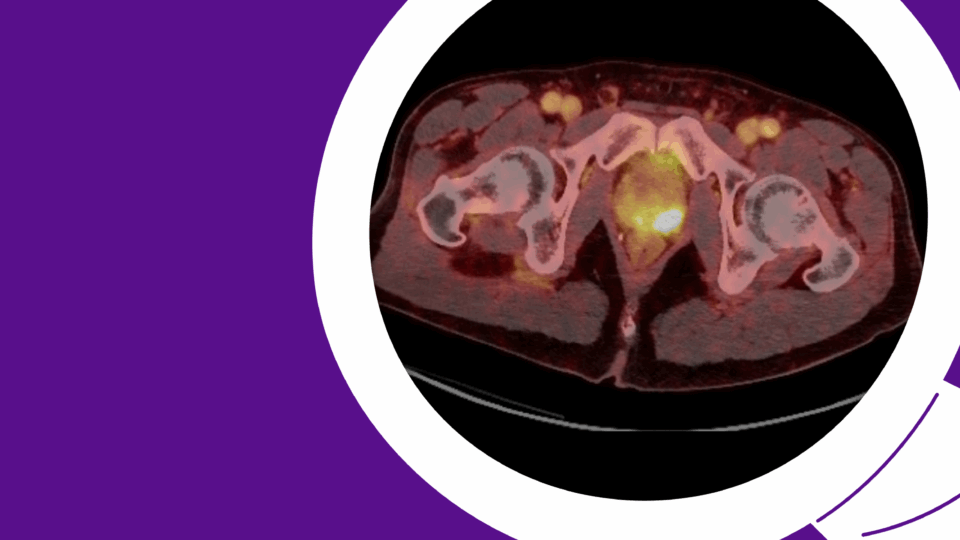
After transrectal sonography confirmed recurrence of the previously aspirated midline prostatic cyst (Figure 2), the patient was diagnosed with partial ejaculatory duct obstruction due to midline prostatic cyst, along with bilateral varicoceles.
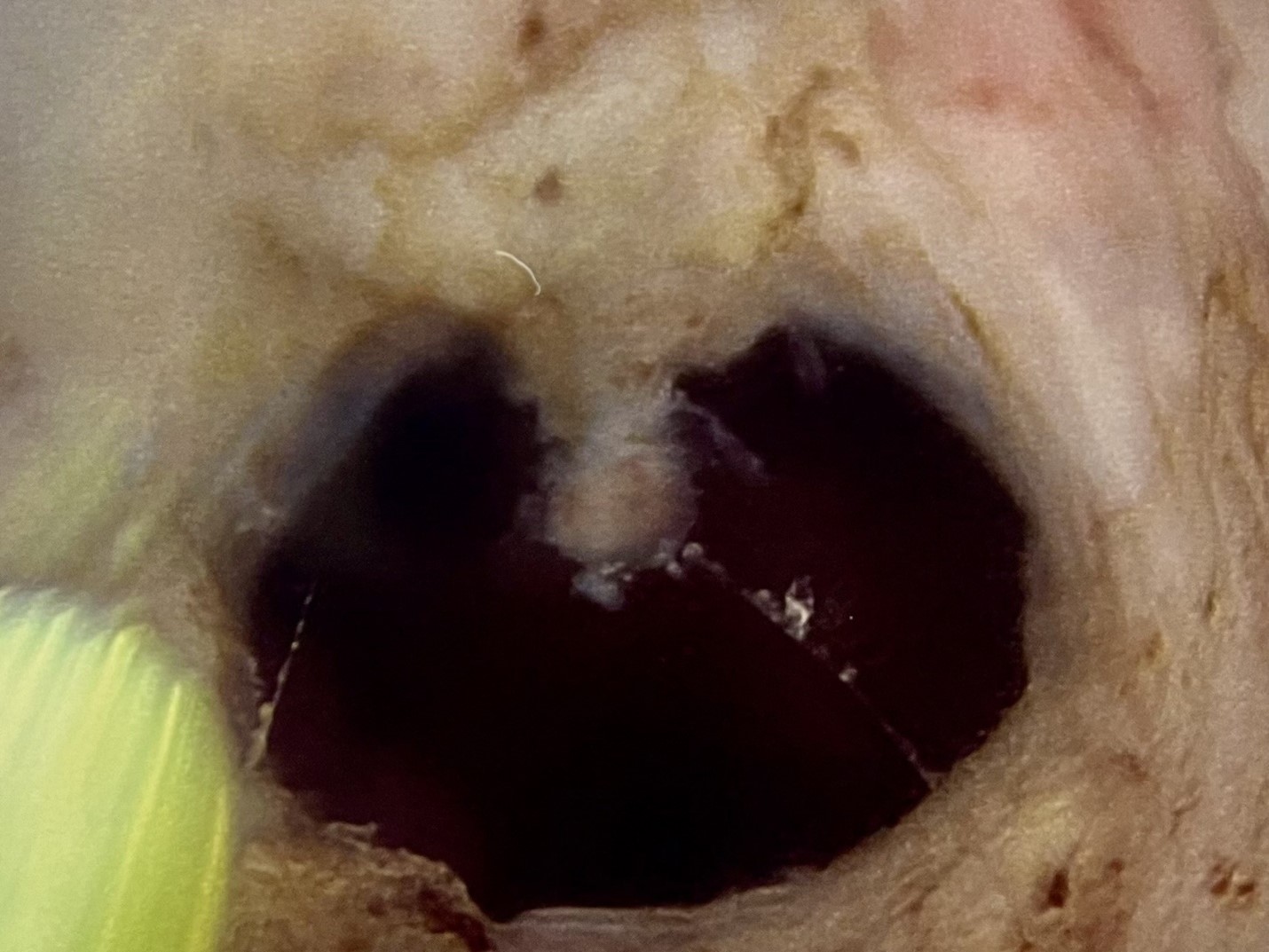
The patient underwent TURED and bilateral microsurgical varicocelectomy. The verumontanum, which had a typical appearance that was full and bulbous, was resected using pure cutting current using a conventional resectoscope. Flow of milky-appearing fluid from the open ducts was seen after the resection. Intraoperative appearance of the verumontanum before and after TURED are shown below (Figures 3 and 4).
Following the procedure, the patient had complete resolution of the ejaculatory pain with increased ejaculate volume. He remained asymptomatic at a 10-month follow up. Semen analysis showed a normal volume ejaculate (2.5 cc) with improved Kruger morphology, normal concentration, and sperm motility.
Discussion
This case demonstrates how TURED can offer rapid and lasting symptom relief for patients with ejaculatory duct obstruction. TURED is minimally invasive and highly effective, addressing both fertility concerns as well as discomfort related to ejaculation and urination. The procedure provides durable outcomes, making it a rewarding option for patients.
Ejaculatory duct obstruction is a rare cause of male infertility that is diagnosed in 1 to 5 percent of infertile men.1 The condition may be congenital or acquired, with the latter typically due to post-inflammatory scar formation in the prostate or seminal vesicle calculi. Congenital causes are attributed to ejaculatory duct atresia or stenosis and utricular cysts. Utricular cysts have been historically referred to as Müllerian (paramesonephric) duct cysts. However, immunohistochemical studies have shown evidence that the utricle is not a Müllerian duct remnant and instead has a distinct origin from the dorsal wall of the urogenital sinus.2,3
Cases of partial ejaculatory duct obstruction may progress to complete obstruction and diagnosis may be challenging, requiring a high index of suspicion.3 Although vasography can provide a definitive diagnosis, transrectal sonography with a 7 MHz probe alone is sufficient to establish the diagnosis, as it is less invasive and highly reliable.4 Our patient met two of the three typical indications criteria for intervention and treatment (infertility, ejaculatory pain, and hematospermia).
Initially described for treatment of ejaculatory duct stenosis more than 50 years ago, TURED is performed using standard or pediatric resectoscopes under general or regional anesthesia using cutting current to minimize scarring and restenosis of the ejaculatory ducts. Since many patients undergoing the procedure are diagnosed during infertility workup and are younger, with smaller prostates, special attention should be paid to avoid bladder neck, rectal, or sphincteric injuries when resecting the verumontanum.3 Although use of the O’Connor drape for seminal vesicle palpation has been described, I have not found this to be necessary in the vast majority of cases.
Ejaculation may resume in one week. Urethral catheterization for 24 hours after the procedure is optional.
In my experience, relief of ejaculatory pain is usually immediate, but it may take a few months to achieve maximal ejaculatory volumes and improved semen parameters. The vast majority of appropriately selected patients with low volume azoospermia due to ejaculatory duct obstruction will have a dramatic improvement in ejaculatory volume and semen parameters, but 10 to 15 percent may convert to normal volume azoospermia due to more proximal or epididymal obstruction.3
Patients with partial ejaculatory duct obstruction will similarly see significantly improved ejaculate volumes, though a small percentage may become azoospermic due to postoperative ejaculatory duct fibrosis and are well advised to cryopreserve sperm prior to the procedure.3,5
References
- Pryor JP, Hendry WF. Fertil Steril. 1991;56(4):725-730. DOI.
- Shapiro E, et al. J Urol. 2004;172(4 Pt 2):1753-1756. DOI.
- Modgil V, et al. Nat Rev Urol. 2016;13(1):13-20. DOI.
- Belker AM, Steinbock GS. J Urol. 1990;144(2 Pt 1):356-358. DOI.
Xu B, et al. BJU Int. 2011;108(2):263-266. DOI.