Referral Notes:
- Addressing the risk associated with placenta accreta requires early imaging-based diagnosis and comprehensive, highly coordinated care.
- NYU Langone’s new program emphasizes the collaboration and evidence-based tools needed to plan for expected deliveries as well as medical emergencies.
- Program co-directors also plan to pursue research and postdelivery uterine preservation to improve patient outcomes.
On a Saturday afternoon several weeks before her due date, a pregnant woman with a history of two prior cesarean sections was rushed to NYU Langone Hospital—Brooklyn with heavy bleeding. She’d previously received a diagnosis of placenta accreta spectrum (PAS) disorder from maternal–fetal medicine specialist Shilpi S. Mehta-Lee, MD, after imaging revealed a placenta previa and evidence of placental vessels within her uterus and her bladder.
In patients with PAS, attempting to separate the placenta from the wall of the uterus can trigger massive and life-threatening hemorrhage. In this case, the prenatal bleeding that prompted the patient’s presentation to the hospital was likely due to the dilatation of her cervix from premature labor, exposing the placental bed in the setting of the placenta previa.
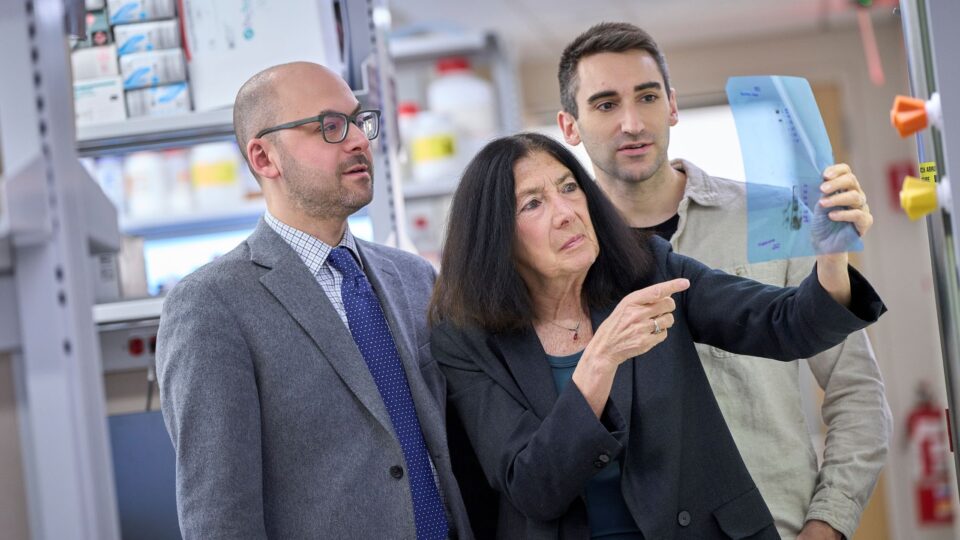
The multidisciplinary care team, including Lindsey Buchin, MD, Rebecca H. Jessel, MD, and Brian D. Taussig, MD, quickly mobilized and helped deliver a premature but healthy baby via cesarean section. Gynecologic oncologist Fady Khoury Collado, MD, was then able to safely perform a complicated hysterectomy, removing the uterus and the placenta while preserving the integrity of the patient’s bladder despite placental invasion.
The resolution of this complex case exemplifies the systematic approach to imaging, early diagnosis, and coordinated care offered by NYU Langone’s new Placenta Accreta Diagnosis and Treatment Program.
“We’re giving every physician who’s practicing maternal–fetal medicine the tools by which to identify this disease early on, and then make a plan for a safe delivery.”
Shilpi S. Mehta-Lee, MD
“Through this program, we’re giving every physician who’s practicing maternal–fetal medicine the tools by which to identify this disease early on, and then make a plan for a safe delivery,” says Dr. Mehta-Lee. “It’s really a quality initiative from the get-go.”
From Early Diagnosis to Coordinated Care
One of the biggest risk factors for PAS is a history of cesarean sections. For women like the presenting patient, with placenta previa and a history of two prior cesareans, the risk of placenta accreta is as high as 40 percent. “With an estimated incidence of 1 in every 272 pregnancies, we’re seeing an exponential rise in the condition, tracking with the rising rate of C-sections,” says Dr. Jessel.
Building on NYU Langone’s long-standing success in maternal and perinatal care, the new program aims to not only boost early diagnosis for PAS and strengthen the necessary care coordination across multiple specialties, but also improve long-term health outcomes.
“We have a top-notch multidisciplinary team with the experience and expertise to handle patient referrals for what can be an exceedingly complicated and high-risk condition,” says Dr. Khoury Collado, who with Dr. Jessel serves as a program co-director.
“We have the experience and expertise to handle patient referrals for what can be an exceedingly complicated and high-risk condition.”
Fady Khoury Collado, MD
A central focus of the program is on educating and training staff, including the maternal–fetal medicine team and ultrasound technologists, on evidence-based diagnostic and treatment protocols. Early imaging and diagnosis, in turn, allow for two comprehensive care plans: one based on everything proceeding as expected, and a second that accounts for various what-if scenarios, says Dr. Mehta-Lee. “You always have both. But without identification, we can’t save women’s lives,” she says.
To manage PAS, doctors generally deliver the baby via a planned C-section, being careful not to disrupt the placenta. They leave the placenta attached to the uterus and then remove it and the entire uterus together via a hysterectomy.
“Despite that, it’s still considered a high-risk surgery with a high risk of bleeding, requiring several teams to work together,” says Dr. Khoury Collado.
The new program is helping to bolster that essential coordination of prenatal care and surgical planning leading up to the day of delivery. At NYU Langone, multidisciplinary care for patients with PAS routinely involves neonatologists, an experienced nursing team, maternal–fetal medicine specialists, obstetrical anesthesiologists, gynecological oncologists, interventional radiologists, urologists, and the blood bank. “It really does take a village,” Dr. Jessel says.
A Launchpad for Improving Outcomes
Initial sites for the program include NYU Langone Hospital—Brooklyn and Tisch Hospital in Manhattan, with plans for expansion across NYU Langone. As a trauma center, NYU Langone—Brooklyn has ready access to blood supplies and trauma surgeons, Dr. Mehta-Lee emphasizes, allowing it to offer emergency PAS care to a highly diverse patient population. The new program is designed to assess the care team’s needs and ensure rapid, reliable access to these trauma tools and services.
“We want to develop a systematic approach to imaging and early diagnosis, and a launchpad to help push the field forward.”
Rebecca H. Jessel, MD
As a long-term goal, Dr. Khoury Collado hopes to further improve patient outcomes by increasing the potential for uterine preservation. “Removing the uterus has a lot of psychological and physical health–related consequences. Avoiding that removal is a goal we think we can achieve in some cases,” he says.
In the meantime, the co-directors plan to incorporate an academic research arm to better understand and characterize the disorder.
From the clinical side, they hope to involve NYU Langone’s mental health services and a community health worker or patient navigator to guide patients through the complicated diagnosis and multistep care process. “We want to develop a systematic approach to imaging and early diagnosis, and a launchpad to help push the field forward,” Dr. Jessel says.