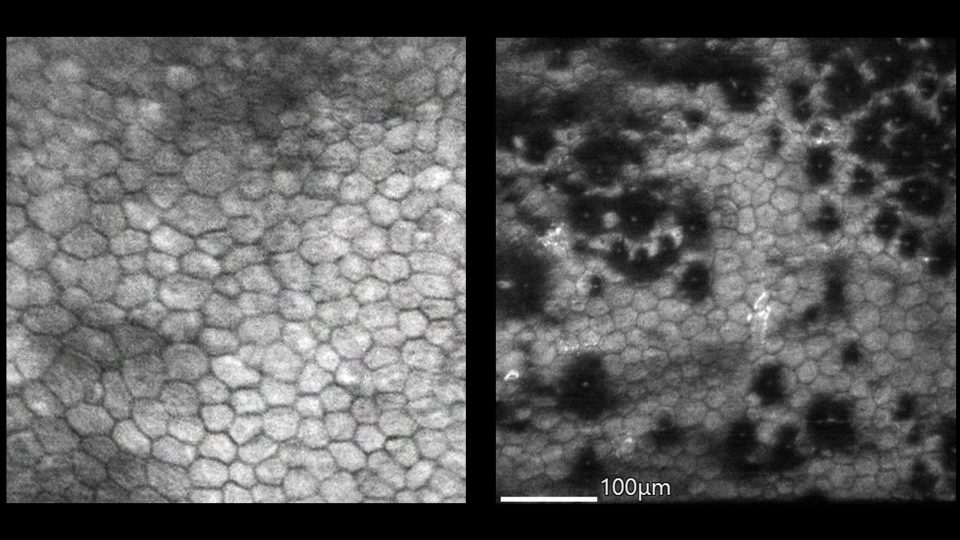
Keratoconus is one of the leading indications worldwide for corneal transplant. As the disease progresses, the cornea undergoes progressive thinning and begins to protrude, causing irregular astigmatism and gradual vision loss.
People tend to develop keratoconus in their teens and 20s after the visual system has matured, says Ann Ostrovsky, MD, a clinical assistant professor of ophthalmology and director of the keratoconus program at NYU Langone Health. “Visual rehabilitation in patients with keratoconus should be possible in most cases since the visual potential of the eye is normal.”
Dr. Ostrovsky and colleagues are advancing keratoconus treatment using topography and tomography imaging modalities to diagnose early-stage disease, as well as collagen cross-linking to halt progression. “Rigid contact lenses can improve vision, but do not prevent disease progression. Advanced disease can result in corneal scarring and frequently requires transplant for visual rehabilitation,” she says.
Shukti Chakravarti, PhD, a professor of ophthalmology and pathology, is a cell biologist researching the pathogenesis of the disease. Together, Dr. Ostrovsky and Dr. Chakravarti are collaborating to understand the fundamental causes of keratoconus.
“We have families where several members are affected,” Dr. Ostrovsky says. “Those with certain systemic conditions, such as Down syndrome, connective tissue disorders like Marfan syndrome, and collagen vascular diseases, have a higher prevalence. Additionally, severe ocular allergy, blepharitis, and forceful rubbing can aggravate this condition.”
Investigating Genetic Components
Dr. Chakravarti began researching keratoconus because of her interest in extracellular matrix (ECM)–related pathologies of the cornea. “Initially, we were just looking for ECM changes and their effects on cell-to-cell communication. But a strong genetic component in keratoconus is undeniable,” she says.
“It is increasingly being appreciated that in a majority of patients, keratoconus is a polygenic, multifactorial disease. In that sense, it’s different from other diseases of the cornea that are caused by a handful of genes, like Fuchs dystrophy. Thus, studying keratoconus requires multiple approaches,” Dr. Chakravarti adds.
“In a majority of patients, keratoconus is a polygenic, multifactorial disease. In that sense, it’s different from other diseases of the cornea that are caused by a handful of genes.”
Shukti Chakravarti, PhD
In a DNA sequencing study of 11 families affected by keratoconus, the researchers found potentially pathogenic variants in 8 different genes. Some were related to ECM integrity, which confirmed the investigators’ suspicion that ECM genes are important in keratoconus.
Patients with keratoconus with no obvious family history are also being recruited at the NYU Langone Eye Center for genomic studies. The researchers hope the pathogenic changes unraveled from discarded corneal tissues will provide clues about candidate genes in the isolated keratoconus patients.
Focus on Oxidative Stress
Dr. Chakravarti and colleagues have performed RNA sequencing and proteomic studies of discarded corneas from patients with keratoconus, identifying potential biomarkers and decreased antioxidant responses. “We think that unresolved oxidative stress impacts structural proteins that protect the eye’s integrity,” Dr. Chakravarti says.
She points to the potential diagnostic value of this discovery in keratoconus screening. “We realized that some of the oxidative stress byproducts show up in the tears; we are hoping to develop these as biomarkers or predictors of disease severity.”
There is utility in understanding the genetics, she adds, not only for stratifying patient risk, but in clinical scenarios. “For example, people who have a genetic predisposition to keratoconus should carefully be counseled about LASIK surgery because their corneas may already have an underlying structural weakness.”
Promoting Early Diagnosis
Dr. Ostrovsky is focused on raising awareness among pediatricians and eye care specialists to promote early diagnosis of keratoconus, especially in susceptible populations. To further this effort, she helped to establish NYU Langone’s multidisciplinary Down Syndrome Program, which includes ophthalmology.
In a recent article for the American Academy of Pediatrics, Dr. Ostrovsky outlines the hurdles in diagnosing disease in patients with Down syndrome. “These cases can be quite challenging because children with Down syndrome frequently don’t complain of vision loss,” she says, “and vision screening as well as obtaining quality tomography images are challenging due to patient cooperation.”
“Basic topography equipment is widely available but interpreting the results can be complicated. In subtle cases, it may be helpful to have a consultation with a cornea specialist.”
Ann Ostrovsky, MD
As for the future, Dr. Ostrovsky says there is still work to do regarding screening paradigms for eye care professionals. “Basic topography equipment is widely available but interpreting the results can be complicated. In subtle cases, it may be helpful to have a consultation with a cornea specialist. This is where biomarkers can also be helpful.”